When you encounter someone on the street experiencing homelessness or hear about an individual overdosing in the city, do you perceive them negatively? In this video, DESC Opioid Treatment Network (OTN) Nurse Supervisor Jeremy Hoog challenges misconceptions about those experiencing homelessness or struggling with substance use disorders. Jeremy was one of a panel of experts who recently spoke about substance use and harm reduction at DESC’s event, “Mission Possible: Adaptive Solutions to Homelessness.” Other panelists included DESC Executive Director Daniel Malone; Co-Director Harm Reduction Research & Treatment (HaRRT) Center, UW, Seema L. Clifasefi PhD, MSW; DESC Deputy Director for Strategy Nicole Macri; and Director of King County Department of Community and Human Services Kelly Rier.
Our Impact
ORCA Center will provide quick stabilization and resources following overdose





Determined to save lives, a multi-agency partnership will fight the fentanyl crisis with a new strategy beginning early-to-mid 2025. That’s when DESC is expected to open a $12 million Opioid Recovery & Care Access (ORCA) Center on the second floor of the Morrison, at 517 Third Avenue.
Here, people who overdose in King County will be stabilized, receive care, start on buprenorphine or methadone as medically appropriate, connect to resources to continue their recovery, and eat, sleep and shower in safety for their brief stay. People with an opioid use disorder who have not recently overdosed will be able to walk in during certain hours to discuss starting on a medication treatment.
The idea for such a center originated from Dr. Caleb Banta-Green, research professor at the University of Washington Addictions, Drug and Alcohol Institute (ADAI), through conversations with leaders at the Seattle Fire Department, who often are called to respond to individuals experiencing an opioid overdose in the field. UW ADAI partnered with DESC to design and advocate for the ORCA center and will be conducting evaluations of its implementation and effectiveness once services begin.
Thanks to a private donation, an award from the city of Seattle and grants from King County and Washington state, DESC is able to convert the former main emergency shelter in the Morrison into a behavioral health clinic featuring opioid use disorder stabilization services and other mental health and substance use disorder treatment services relocated from DESC’s 216 James Street facility.
“It’s great to have this project continue to move forward,” said DESC Executive Director Daniel Malone. “We are working toward a completion in the first few months of next year.”
“The ORCA Center adds another important link to our continuum of services for people who experience drug overdoses and who have opioid use disorder,” Daniel said. “By providing much-needed treatment such as medications for opioid use disorder, as well as access to harm reduction supplies, education and other services, we aim to prevent the next overdose and cut down on emergency room use.
“This will be one of many services and strategies designed to reduce fatal overdoses and fentanyl harm and increase well-being in the city and the county. Thank you to our multiple city, county and regional partners in crisis and behavioral health services who share those priorities and goals. And thank you to the City of Seattle, King County, Washington state and a generous private benefactor without whose investments this center wouldn’t be possible.”
Additional needs DESC has identified include the creation of dedicated emergency housing for people who use the ORCA Center but do not have stable housing to return to.
DESC Medical Director Richard Waters, M.D., said the center is “one important and notable but small piece in the landscape of services and strategies in reducing overdose deaths and the harms of fentanyl in the city and county. Its success hinges on the success of longitudinal outpatient teams to continue MOUD (Medication for Opioid Use Disorder) and other supports to the well-being of individuals that ORCA will serve.”
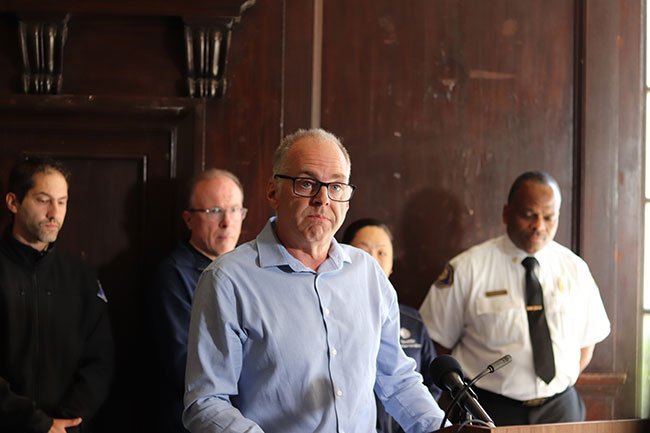
In a press conference at DESC on May 9, Seattle Mayor Bruce Harrell announced the city’s commitment of $5.65 million toward the ORCA Center. The award is part of a $27 million investment supporting Harrell’s executive order addressing the drug crisis in Seattle. Evergreen Treatment Services (ETS), an important DESC partner whose services include a mobile clinic providing methadone treatment, received a $1.35 million award from the city.
The media event brought together all the partners in this project:
- University of Washington–Addictions, Drug and Alcohol Institute (ADAI)
- Public Health–Seattle and King County
- King County Behavioral Health and Recovery Division (BHRD)
- Seattle Fire Department
- City of Seattle Human Services Department
- Harborview Medical Center
- Evergreen Treatment Services
Why do we need a place like the ORCA Center?
New medications and approaches show promise. Long-acting injectable buprenorphine medications seem to strongly increase a person’s ability to continue with treatment, but it’s difficult to provide to the population we serve if they don’t have safe places to be and to recover. People will be able to receive this form of rapid care and treatment in a physical space such as the ORCA Center.
The ORCA Center will also provide
- Peer Specialists to connect individuals with service options
- Medical staff to support starting MOUD
- Case management staff who offer low-barrier harm reduction-oriented care, and connection to outpatient behavioral health and other needed resources
- Basic need accommodations during treatment
- Access to continued care/treatment for MOUD and other behavioral health services.
What are our goals for the ORCA Center?
- Lower fentanyl mortality rates for our client population
- Increase MOUD initiation rates
- Lengthen the time people stay on MOUD
- Cut down ER use
- Enhanced research and best practices related to long-acting injectable Medications for Opioid Use Disorder (MOUD).
Opioid Treatment Network removes treatment barriers to save lives
Tragically, last year in King County, over 1,300 people lost their lives to overdoses. This loss of friends, family and community members is devastating, but a DESC program gives us hope during these difficult times.
Continue reading “Opioid Treatment Network removes treatment barriers to save lives”Annual Report 2022
The figures in this report are for fiscal year January-December 2022, released in July 2023 following annual auditing.
Thanks to DESC housing and shelters, thousands of people slept indoors and not on the streets; a total of 650,262 bednights in 2022!
Continue reading “Annual Report 2022”Annual Report 2021
Annual Report 2021
The figures in this report are for fiscal year January-December 2021, released in July 2022 following annual auditing.
Your support saves lives every day
“DESC was a hope in my life when I had no other…Now I have peace and serenity. Peace of mind.”
